BGs & the Birds and the Bees
Diabetes can sometimes be an unwelcomed bystander during sex.
That became alarmingly clear to me once I started wearing a continuous glucose monitor. While it is great to know where I am and where I am going glucose level-wise, a CGM (continuous glucose monitor) sounding off could be coitus interruptus.
Sexual encounters often involve movement and movement can cause fluctuations in our blood glucose levels. This can be further complicated by the very nature of sex as it can vary in duration and intensity. And that can make it difficult to be prepared and stay in range.
Low glucose events can find you prematurely sweaty and in desperate need of glucose tabs or that juice box on the nightstand. It is always best to treat the low. Do not ignore it.
There have been countless times over the years where I have whispered to my husband, I’m sweating more than I should be, let me check my sugars. Only to discover I am low and need to pause to scarf down glucose tabs or have a juice box.
Then comes the need to recover afterwards.
A bad low during sex could potentially derail the encounter entirely, so it is best to be prepared.
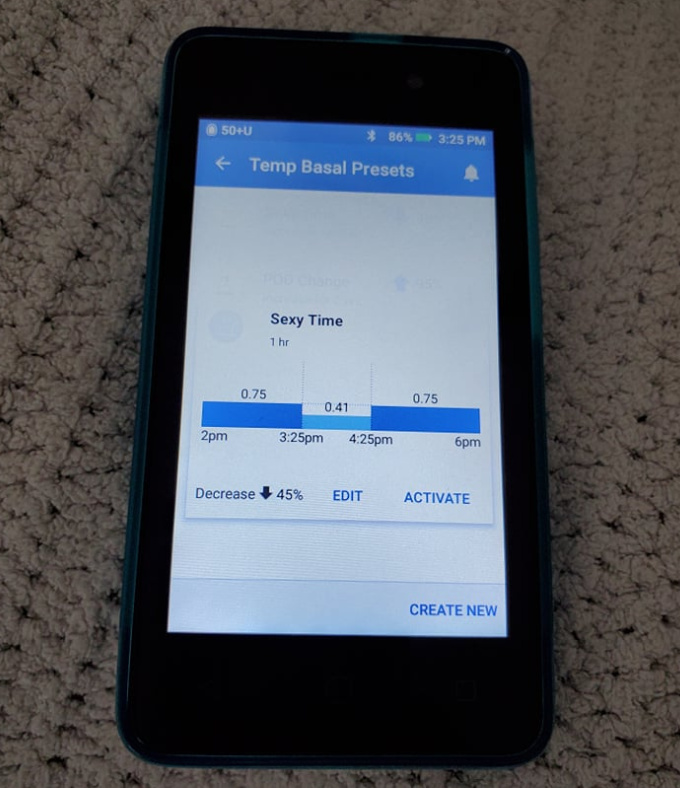
The Omnipod DASH® System allows Temp Basal Presets and I have one specifically for those intimate moments. It has taken years and some crafty calculations to reach this point, but my “Sexy Time” Temp Basal program helps me to be as prepared as possible and limit those interruptions.*
A sexual encounter can also evoke emotions and stress which can cause our blood glucose levels to rise. Those high glucose levels can then lead to thirst and an increased need to urinate...and potentially ruin the mood.
Taking stock of your T1D before sex may feel completely unsexy but open communication with your partner and repetition can help normalize that mid-sexy session glance at your blood sugar levels.
If you need to pause for a snack, invite your partner to nibble alongside you.